Research
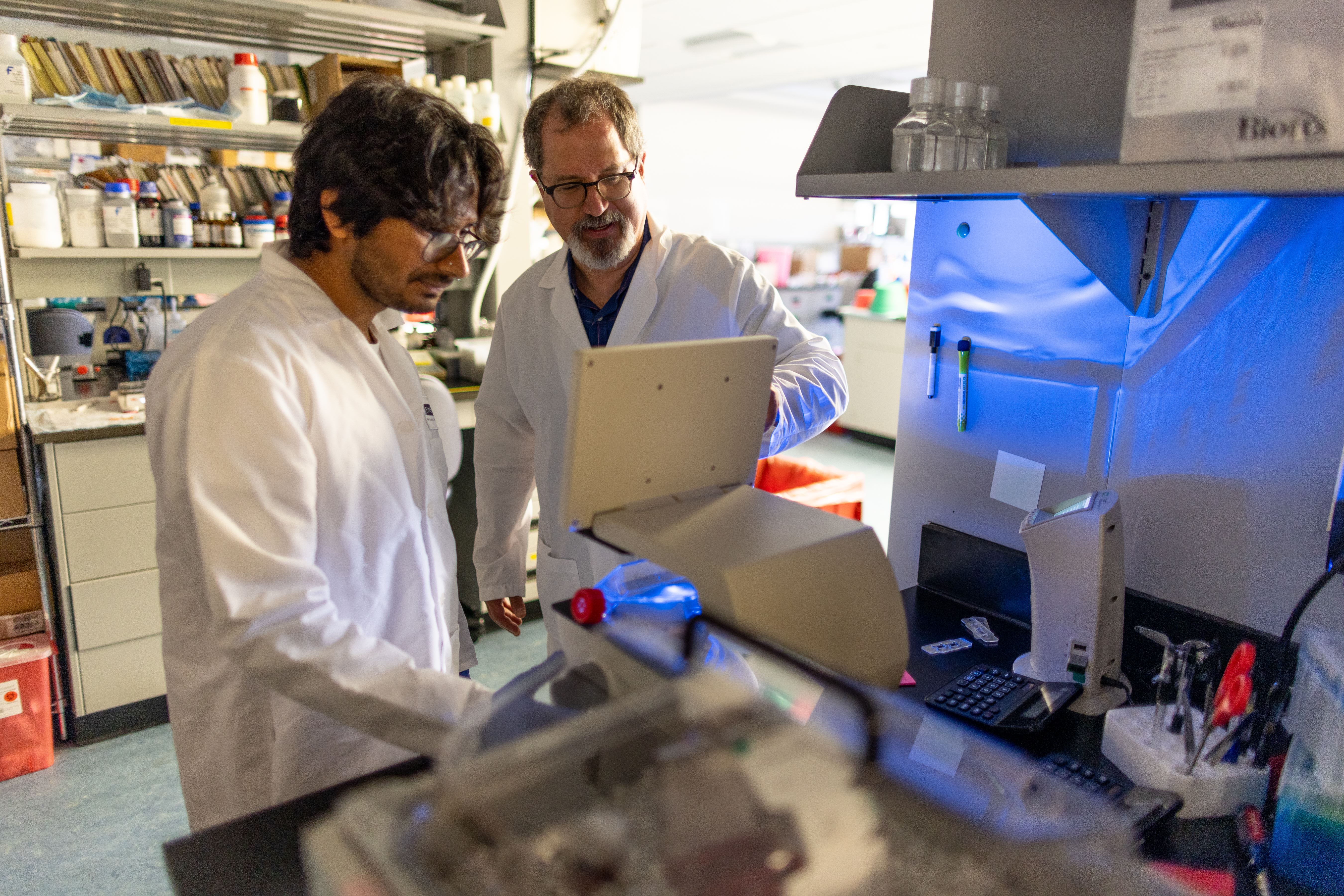
Leading the fight against childhood cancer: Bringing research from the laboratory to the bedside
At CHAM, we are dedicated to improving outcomes for children with cancer and blood disorders. Our cross-disciplinary research model brings together outstanding physicians with internationally-recognized scientists at Albert Einstein College of Medicine to develop our own innovative therapeutics and treatment strategies. We confront highly aggressive forms of pediatric cancer and blood disorders with an equally aggressive push toward advancing the field.
Providing access to clinical trials worldwide
The Pediatric Hematology, Oncology, and Cellular Therapy team at CHAM is at the forefront of clinical research and development in the field of childhood cancer and blood disorders, actively involved in defining the next generation of treatment. To do this, our physician-scientists are developing new treatments in their research labs and we work closely with other leading children’s hospitals around the world to bring the latest and most promising treatment options to our patients. Clinical trials at CHAM allow our patients to be among the first to try pioneering treatment agents and concepts.
CHAM is an active member of many national and international consortia of pediatric cancer centers dedicated to advancing treatment for children with cancer by combining global resources and expertise for clinical trials. We participate in studies through the Children’s Oncology Group (COG) and National Institutes of Health (NIH), Dana-Farber Cancer Institute, the National Pediatric Cancer Foundation, as well as industry-sponsored and NIH-supported investigator-initiated clinical trials.
In all areas of research, the CHAM Hematology, Oncology, and Cellular Therapy team is a key player in the ultimate fight — to one day entirely eradicate childhood cancer and blood disorders.