Function: Surgical Procedures We Perform

Selective Tibial Neurectomy
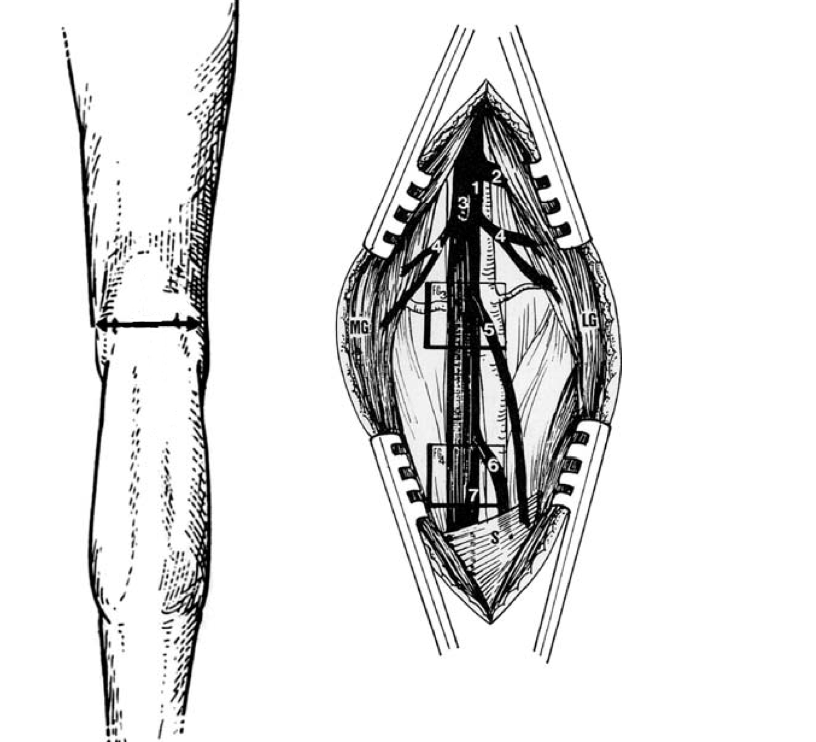
A selective neurectomy, or neurotomy of the Tibial Nerve, refers to exposing the nerve to the calf and foot muscles, and then cutting a portion of the nerve. Before our physicians do so, we conduct tests to determine which of the nerve’s branches are causing the muscle to contract abnormally.
The operation offers the effects of a Botox injection but, unlike Botox, the operation’s effects are permanent and there is no pain after the procedure.
How it works:
Specialists make a cut in the skin behind the knee in order to expose the nerve (as seen in the picture on the right). The branches of the nerve to the calf muscles (numbers 4 and 5) are electrically stimulated, and the strength of the resulting muscle tightening is felt. A portion of these branches is then cut. We then retest the branch to judge whether or not the desired weakening has been achieved.
Why it works:
This operation allows our surgeons to identify exactly which nerve branches are causing abnormal tightening of the calf muscles and partially cuts them. This weakens the calf muscle.
Benefits:
Weakening the spastic or tight calf muscle allows other muscles in the leg to better control its movement. The weakening in the muscle also lessens or eliminates painful contractions and spasms. This weakening is permanent, so no further treatments for calf muscle tightness are usually required.
Possible problems:
As with any surgery, infection and bleeding can complicate healing. When they occur, additional treatments may be needed. Rarely, there may be more or less weakening of the calf muscles than is desired.
Other ways to manage the condition:
Oral medications or BOTOX, phenol or ethanol injections can also treat tightness in the calf muscles. The tendons or leaders of the calf muscles can also be lengthened, so that the tight muscle does not pull as forcibly on the ankle joint.
Intrathecal Baclofen
Intrathecal Baclofen refers to the delivery of the anti-hypertonia drug Baclofen directly into the spinal fluid space of the spine. The objective is to obtain a higher amount of the drug at its treatment target site within the spinal cord. At the same time, we can avoid high drug concentrations at higher levels of the central nervous system (the brain and upper spinal cord), where it can cause undesired side effects (including lethargy and respiratory depression).
How it works:
An implanted drug reservoir with a pump is used to deliver a small amount of the drug via a thin catheter unto the spinal fluid space in the upper, mid- or lower back.
Why it works:
When it is delivered this way, typically the concentration of the drug is 100 times higher in the lower (back?) than it is in the brain. This allows for a much high drug concentration to work at the target sites within the spinal cord, without the worry of undesired side effects. The concentration achieved is much higher than can be accomplished when the same medication is taken by mouth.
The CHAM surgeon who implants the pumps for this treatment is at the forefront of the use of this procedure. He was part of the initial FDA trial of programmable infusion pumps for delivery of intrathecal baclofen in children in the mid 1990s, when this treatment was first introduced for managing hypertonia in children.
Selective Neurectomy
Selective neurectomy refers to the cutting of a portion of a peripheral nerve in a “selective” or directed fashion, in order to preserve a distinct part of the nerve. Our Center is one of the few in North America that offers this procedure for the treatment of muscle spasticity or stiffness.
How it works:
The selective neurectomy surgeon at Function exposes the nerve at a point where it is giving off branches to a muscle whose tightness is contributing to a disability, stimulating each of the nerve’s branches to that muscle and then cutting roughly 70% of the branches that are causing the greatest degree of contraction in the muscle.
Why it works:
This technique has several advantages. By exposing the branches going to the targeted muscle and working only with them, we can preserve the portion of the nerve containing fibers that deliver sensation back to the brain. By stimulating each branch, the physician can determine which branches cause the greatest force of contraction and focus solely on them. Lastly, by stimulating each branch, some functioning nerve supply will be maintained to the muscle, so that it will not become completely paralyzed.
Benefits:
The selective neurectomy can be performed on any nerve giving branches to a muscle where stiffness or spasticity is causing functional problems and/or pain.
To assess the impact of decreasing the muscle’s nerve supply, our specialists at the Center commonly give a reversible nerve injection to the nerve in question at a point where it is giving off branches to a problematic muscle. The solution used for these injections is usually BOTOX or botulinum toxin. The effect, which usually has an onset within days of injection and lasts several months, is then evaluated to insure that we can achieve the desired outcome by relaxing the muscle. When this is confirmed, our team can employ the selective neurectomy to make the benefit permanent.
Our specialists have performed this procedure on the following nerves:
- Pectoral Nerve
- Median Nerve
- Radial nerve
- Ulnar nerve
- Sciatic nerve
- Pudendal Nerve
- Posterior Tibial nerve
- Obturator Nerve
Selective Dorsal Rhizotomy (SDR)
SDR is a procedure in which our surgeons selectively cut the portion of the sensory nerves of a limb or limbs that are causing spasticity. Rhizotomy is another name for a nerve root or, that portion of a peripheral nerve that lies within the spinal canal between the spinal cord and the nerve’s cell body. Dorsal or posterior refers to that portion of the nerve root that contains the sensory fibers, as opposed to the ventral or anterior root that contains the motor fibers (those fibers that tell a muscle to move). Selective refers to the fact that the cutting is incomplete, and the portion of sensory nerve fibers that are cut is directed by some form of “selection” process.
There are many different criteria used to determine what sensory nerve fibers are cut in this operation. In general, in North America the selection process involves electrically stimulating bundles of sensory fibers and then monitoring the subsequent pattern of muscle contraction in the body that occurs.
There is an expected pattern of muscle contraction that should be seen, depending on which fiber bundle is stimulated. When this occurs, our specialists label the response as “normal.” When muscles other than those expected to contract are seen to do so, we determine the response to be “abnormal.” Lesioning is typically isolated to those sensory nerve fibers whose stimulation causes “abnormal” patterns of muscle contraction.
Our Function surgeon is a pioneer in the use of this procedure. He was the first to perform it in North America and introduced it to Northeastern United States in 1986. He also first introduced the use of multichannel recording of electrical activity in muscles resulting from nerve stimulations for SDR surgeries. In addition, he also participated in the development of nerve mapping procedures to protect the nerve supply to bladder, bowel and sexual organs during the procedure. He has now performed over 300 of these procedures.
Selective DREZotomy
Selective dorsal root entry zone lesioning or Selective DREZotomy, refers to selectively cutting into the spinal cord at the “dorsal root entry zone” in a manner that limits the sensory nerve fibers being cut to the subtypes that delivery sensory information about a muscle’s tightness.
To do this, the incision also must go through the sensory fibers that bring pain and temperature sensation into the spinal cord from a portion of a limb. The procedure seeks to minimize disruption of sensory fibers that bring the sensation of touch and position sense into the spinal cord. This procedure can be considered for treating diffuse spasticity in the arms, where sensation is much more critical for function and where the use of selective dorsal rhizotomy has been found to engender far too great a sensory deficit for the maintenance of limb function.
How it Works:
The selection process involves electrically stimulating the small sensory nerve rootlets as they enter the spinal cord, and then monitoring the pattern of muscle contraction in the body that occurs. There is an expected pattern of muscle contraction that should be seen, depending on which fiber bundle is stimulated. When this takes place, the response is labeled as “normal,” and when muscles other than those expected to contract do so, the response is labeled as abnormal.
Lesioning is typically isolated to the dorsal root entry zone of the spinal cord directly underlying (ventral or anterior to) the sensory nerve fibers whose stimulation causes “abnormal” patterns of muscle contraction.
This technique was introduced in North America in 1998 by a member of the Function team. It has a very limited application, but can be of benefit in specific circumstances where there is diffuse spasticity in the arms that cannot be managed more simply.